Injecting medications into the central nervous system, evaluating the intra-spinal pressure of the cerebrospinal fluid, or sampling the cranial and spinal fluid are some of the most difficult procedures which come under the domain of diagnostics and therapeutics. Multiple neurological diseases as well as certain infectious states need confirmation prior to the start of treatment. Therefore, several processes are employed to evaluate the patients, among which is the technique of lumbar puncture or spinal tap.
What is a lumbar puncture (LP) or spinal tap?
The LP technique was first introduced in 1891 by Heinrich Quincke, a German physician. Lumbar puncture or LP is a medical technique in which the spinal canal is punctured with a needle in order to draw a sample of cerebrospinal fluid (CSF) or to insert a drug into the CNS. This method is also referred to as ‘spinal tap’.

Lumbar puncture technique
Instruments used in lumbar puncture
The single-use, disposable, and sterile lumbar puncture kit includes the following items:
- Lumbar puncture needle with stylet
- Lumbar puncture set i.e. 3-way tap, spinal manometer
- Decontaminants such as 2% chlorhexidine plus 70% isopropyl alcohol or povidone-iodine
- Local anesthetics i.e. 1% lidocaine solution
- Antiseptic solution
- Skin swabs
- 20 and 25-gauge needles
- CSF tubes
- Sterile gown
- Sterile gloves
- Goggles
- Syringe
- Mask
- Dressing
- Sterile field
- Spinal manometer
- Fenestrated drapes
- Marking pen
- Documents including test request forms, patient labels, etc.

The needles used in the process of lumbar puncture for pediatric patients are chosen based on the patient’s age as well as the weight of the child.
| Age of the child | Weight of child (kg) | Length of needle (cm) |
| Neonates and infants | 1 to 5 | 2 |
| 12 to 18 months | 10 | 3 |
| 4 years | 15 | 3 or 4 |
| 6 years | 20 | 4 |
| 9 years | 30 | 4 |
| 12 years | 40 | 5 |
| 14 years | 50 | 5 to 6 |
How to perform lumbar puncture?
The lumbar puncture is performed by following the steps given below:
- Ask the patient to change into the hospital gown before starting the process.
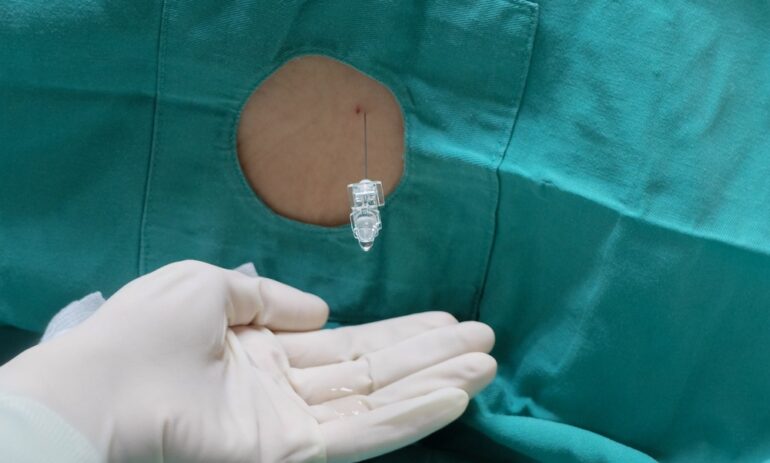
- Once in a gown, ask the patient to lie down preferably on their back with knees drawn up towards the chest.
- Another suitable posture is the sitting position with leaning towards one’s feet.
Positions of the patient suitable for LP procedure
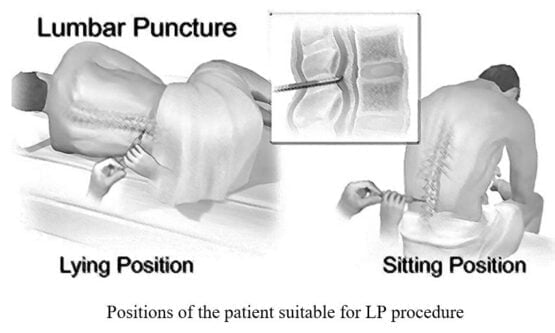
- The procedure is started by injecting a local anesthetic into the puncture site which may cause a stinging sensation for a few minutes.
- In the lumbar region i.e. between the two lower vertebrae named as 3rd and 4th lumbar, a slender needle with a hollow lumen is inserted. The patient may feel pressure being applied to the spinal region.
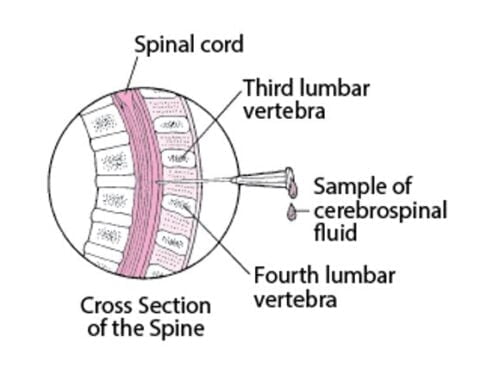
Puncture site for the needle insertion during the LP process
- At this point, the pressure of the CSF is measured and the sample is drawn.
- The needle is drawn out and the injection site is covered with the bandage.
- The patient is treated for pain or bleeding, if necessary.
- It is also advised to avoid strenuous activities for the next 24 hours.
Applications of the lumbar puncture technique
The lumbar puncture technique can be employed for the following purposes:
- In case of suspension of an infection in the brain and spinal cord, along with other inflammatory disorders which may show visible symptoms, it is necessary to take a sample of the CSF to confirm or reject the doubt. Moreover, lumbar puncture is the only technique that can rule out the possibility of meningitis which is a life-threatening condition.
- Trypanosoma brucei infection can also be confirmed by this procedure.
- Diagnosis of the conditions such as subarachnoid hemorrhage, benign intracranial hypertension, or hydrocephalus can easily be done via the lumbar puncture technique. Among these, the symptoms of hydrocephalus can also be relieved once lumbar puncture is done.
- CNS vasculitis, neurosarcoidosis, paraneoplastic syndromes, multiple sclerosis, as well as Guillain-Barre syndrome can also be diagnosed with this technique, although their diagnosis is extremely rare.
- Drugs such as antibiotics, spinal anesthetics, or chemotherapeutic agents can also be administered into the cerebrospinal fluid by employing the lumbar puncture method.
- Radioactive substances or inject dyes can also be injected into the spinal cord to evaluate the flow pattern of the CSF.
Side effects of the lumbar puncture technique
After getting a lumbar puncture, the patient may experience:
- Pain at the site of infection (which is treated with analgesic medications)
- Post-LP headaches (which can be managed by giving an intravenous caffeine injection)
- Nausea
- Numbness
- Cerebral herniation
- Bleeding from the site of injection
- Leakage of cerebrospinal fluid
- Rare incidents of epidural hemorrhage
When not to employ the lumbar puncture technique?
Although the utilization of the lumbar puncture technique in the medical field sounds promising, there are some conditions in which the application of this method can cause harm to the patient instead of benefiting them. The conditions in which lumbar puncture is not recommended include:
- Elevated intracranial pressure
- In patients more than 65 years of age
- In patients with a history of seizures in the near past
- Abnormality in the breathing process
- Elevated blood pressure with a constantly low heart rate
- Low platelet count (lower than 50 x 109/L)
- Infection on the skin near the spinal cord
- Deformities of the vertebral column (can be done but expertise is required)
Conclusion
The lumbar puncture technique is one of the most reliable methods which is used for the diagnosis and sometimes, treatment of CNS disorders. It is an invasive method in which a needle is inserted into the spinal area for the purpose of drawing a CSF sample or for injecting medication into it. The procedure only takes approximately 45 minutes to complete and does not impair the patient’s day-to-day activities by causing severe pain. Although rare incidents of severe after-effects have also been recorded, the procedure is generally considered safe.

PhD Scholar (Pharmaceutics), MPhil (Pharmaceutics), Pharm D, B. Sc.
Uzma Zafar is a dedicated and highly motivated pharmaceutical professional currently pursuing her PhD in Pharmaceutics at the Punjab University College of Pharmacy, University of the Punjab. With a comprehensive academic and research background, Uzma has consistently excelled in her studies, securing first division throughout her educational journey.
Uzma’s passion for the pharmaceutical field is evident from her active engagement during her Doctor of Pharmacy (Pharm.D) program, where she not only mastered industrial techniques and clinical case studies but also delved into marketing strategies and management skills.
Throughout her career, Uzma has actively contributed to the pharmaceutical sciences, with specific research on suspension formulation and Hepatitis C risk factors and side effects. Additionally, Uzma has lent her expertise to review and fact-check articles for the Health Supply 770 blog, ensuring the accuracy and reliability of the information presented.
As she continues her PhD, expected to complete in 2025, Uzma is eager to contribute further to the field by combining her deep knowledge of pharmaceutics with real-world applications to meet global professional standards and challenges.